The urinary incontinence in children refers to the loss or leakage of urine. This situation represents a frequent cause of consultation in paediatric centres.
The urinary incontinence you can:
- Create stress, anxiety, and embarrassment for the children.
- To avoid that enjoy social activities.
- Affect the school performance of a child.
- Generates lost work days for parents.
Causes
There are many reasons why children wet:
- Many children do not want to miss the fun activities to go to the bathroom.
- Some children wet their only two or three times a day; they are just too busy to go to the bathroom until it's too late to reach the bathroom in time.
- Other children have contractions uncontrolled and involuntary bladder (Overactive muscle of the urinary bladder or detrusor) , that make them feel that they need to go to the bathroom “you Anymore, now!”
- Some children do not empty your bladder completely when you go to the bathroom, leaving residual urine.
Dysfunction of evacuation
Means your child can't completely empty your bladder.
- In a normal cycle, your son's bladder stretches easily when it is filled with urine, and then it collapsed completely during the evacuation.
- There must not be premature contractions of the bladder or increased pressure as it is filled.
- During the phase of normal bowel movement, there must be a complete relaxation of the muscle of the external urethral sphincter, so that the urine is released from the bladder to flow smooth and complete, without interruption, as the bladder is empty.
- A flow interrupted or intermittent urine or incomplete emptying are the causes of voiding dysfunction or evacuation.
- There can be an association with intestinal disorders, such as Constipation and/or Fecal Incontinence.
Complementary studies:
- Record journal urinary and calendar
- Uroflowmetry with electromyography perineal.
- Ultrasound kidney and bladder with measurement of residue postmiccional
Treatment for Lower Urinary Tract Symptoms:
Nuestro Centro está dedicado al tratamiento, manejo de niños con urinary incontinence and some intestinal disorders. Will work with you and your child to help you understand why you get wet urine or soiled his underwear and recommend a treatment plan, so that it does not require the use of protective / diapers and protect your tree urinary.

The necessary steps to control urinary incontinence in children include:
- Urinating on a routine schedule of every two to three hours.
- Identifying the constipation and the constipation behind.
- Increase the amount of water consumed during the day.
- Avoid drinks that irritate the bladder: caffeine, carbonation, citrus juices with stimulants and sports.
- Appropriate position on the toilet.
- Training with biofeedback Biofeedback: a noninvasive way to teach children how to relax the pelvic floor muscles so that they can empty the bladder completely. This program will require several visits or sessions in a given period. The child comes in contact with a program computed friendly with stories and figures for children that will guide you to achieve your goals, continually accompanied by Nurses and trained Specialist. It is necessary and important for the willingness and the motivation in children to that a program has acceptable results.
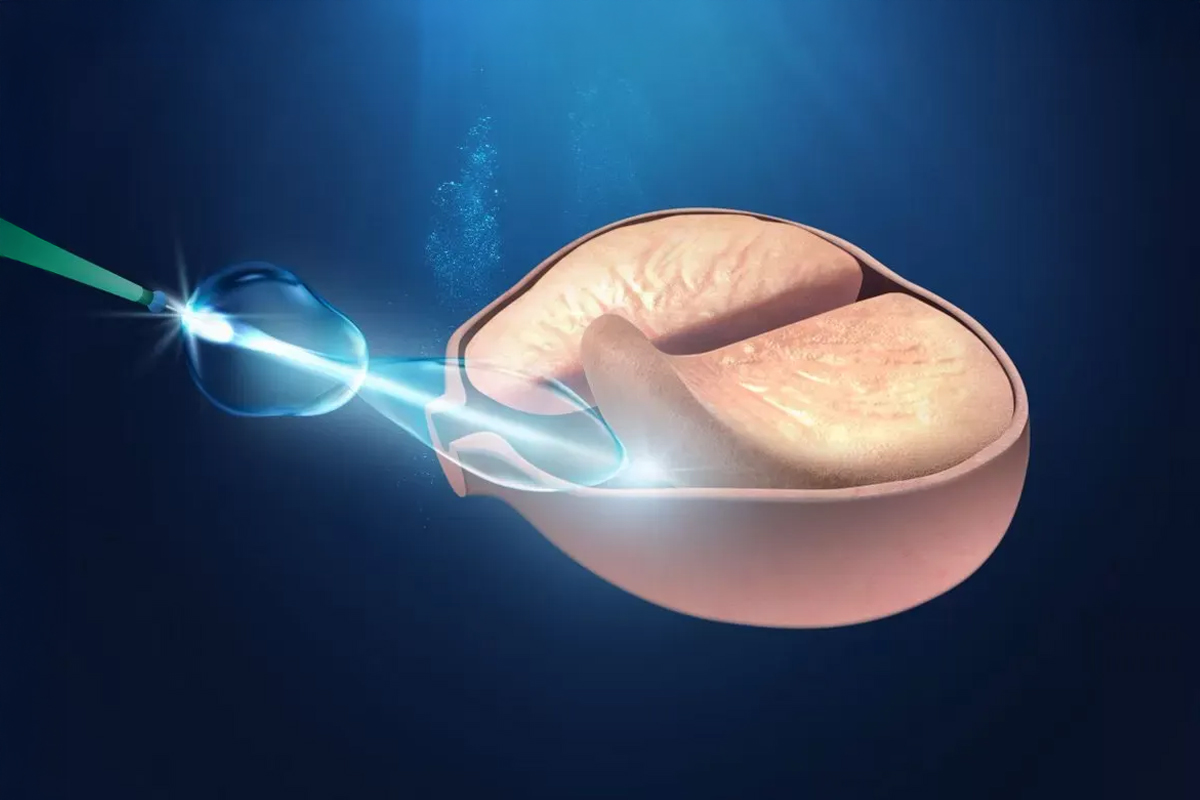
- Neuromodulación / Estimulación Nerviosa Eléctrica Transcutánea: La neuromodulación evoca a la modificación de la actividad de la vejiga y los esfínteres, gracias a un estímulo eléctrico controlado de muy baja intensidad. Es una terapia “No medicamentosa”, que se utiliza de forma segura, en niños, para diversos trastornos funcionales de las vías urinarias bajas y también del intestino. Al prescindir de drogas, se desprende la ventaja de evitar efectos indeseables derivados del uso de medicamentos. Este método utiliza corriente eléctrica de baja frecuencia e intensidad, aplicada “superficialmente” con electrodos autoadhesivos en zona lumbar. Es un procedimiento indoloro y el niño puede distraerse con apps, tablets o libros. Indicaciones: Sobreactividad del músculo vesical o detrusor, constipación y LUTS en “pacientes neurológicamente sanos”, como segunda línea de terapia refractarios a Uroterapia estándar y a medicación anticolinérgica. Este programa requerirá varias visitas o sesiones en un periodo determinado.