El cáncer de próstata es el más común de los cánceres en la población masculina, representando casi un 23%, de los nuevos tumores diagnosticados en los varones. El riesgo de padecer cáncer de próstata está ligado con la edad, muy pocos casos son diagnosticados en varones por debajo de los 50 años y un gran porcentaje de los diagnósticos ocurren en hombres mayores de 70 años. Los hombres con antecedentes de historia familiar con cáncer de próstata, deberían comenzar sus controles a los 45 años.
In recent years there has been an increase in the detection of prostate cancer through the use of the analysis of blood prostate specific antigen (PSA) and by surgery bph where you submit material to analyze pathological anatomy and arises the diagnosis.
– Diagnosis and staging of prostate cancer –
The consultation of the specialist of Urology for prevention is beginning to be installed in the population, with the possibilities of preventative medicine. Which is achieved with the query and the realization of the different complementary studies are necessary, according to the Urologist to consider for each patient.
- Review / digital rectal exam: it consists of a test by which the Urologist inserts a finger into a glove, lubricated into the rectum and feels the prostate through the rectal wall for lumps or abnormal areas.
- Prostate-specific antigen (PSA): prueba de laboratorio que mide las concentraciones del PSA en la sangre. Esta es una sustancia producida mayormente por la próstata que se encuentra en mayor cantidad en la sangre de los hombres que tienen cáncer de próstata. Cabe mencionar, que también, el resultado del PSA puede ser elevada en los hombres que sufren una infección (Prostatitis) o una inflamación de la próstata, o que tienen una hiperplasia prostática benigna (HPB).
- Transrectal ultrasound: a procedure in which is inserted into the rectum a probe to examine the prostate.
- Prostate biopsy: the removal of cells or tissues to observe them under the microscope. The Pathologist examines the sample for cancer cells and determine the Gleason score. The Gleason score ranges from 2 to 10, and describes the biological activity and the possibility that the tumor will spread. The lower the score, the lower the probability of spread of the tumor. The Transrectal Biopsy was the more traditional method and consists in the removal of tissue from the prostate by inserting a thin needle through the rectum into the prostate. This procedure is done using transrectal ultrasound to guide the needle.
– Magnetic resonance imaging Multiparamétrica and Biopsy –Fusion
Changes in the paradigm of diagnosis in prostate cancer.
The recent study called PRECISION (Prostate Evaluation for Clinically Important disease: Sampling using Image-guidance Or Not?) published in the renowned journal The New England Journal of Medicine has shown results that impact the diagnosis of prostate cancer. In this international study, 500 men with suspicion of prostate cancer due to increased PSA (Prostate Specific Antigen) were separated into two groups.
Para el grupo 1 se aplicó el método de diagnóstico tradicional: una biopsia prostática transrectal guiada por ecografía, con la toma de 12 muestras. En el caso del grupo 2, la evaluación se basó en los hallazgos obtenidos mediante una Resonancia Magnética Nuclear Multiparamétrica de próstata (RMNmp). Cuando esta resonancia mostraba resultados anormales, se procedía a realizar una biopsia prostática por FUSIÓN, utilizando un software que integraba las imágenes de la resonancia con las de la ecografía, y se extraían muestras exclusivamente de las zonas sospechosas. Cuando esta resonancia mostraba resultados anormales, se procedía a realizar una biopsia prostática por FUSIÓN, utilizando un software que integraba las imágenes de la resonancia con las de la ecografía, y se extraían muestras exclusivamente de las zonas sospechosas.

El objetivo primario buscado en este estudio fue la evaluación de la tasa de detecciónn de cáncer de próstata clínicamente significativo; y dentro de los objetivos secundarios se incluyeron la tasa de detecciónn de cáncer clínicamente insignificante (el cual se define como una enfermedad limitada al órgano con un volumen tumoral <0,5 cm3, con puntuaciónn de Gleason 6, cuyo tratamiento no es necesario ni generará beneficios en los pacientes).
In Group 1 of the biopsy traditional, the detection rate of cancer clinically significant was 26%, and the detection rate of cancer clinically insignificant was 22%. In Group 2, the fusion with Mri, the detection rate of cancer clinically significant in patients who will require treatment increased approximately double with 38% and the detection rate of cancer insignificant decreased to 9% by avoiding to treat cancers that do not require it.

Therefore, despite the fact that more than a quarter of the men in the way of Resonance, in reality, they avoided a biopsy, the detection rate of prostate cancer clinically significant was much higher in this arm. In addition, the rate of detection of cancer clinically insignificant was much lower (i.e., they reduced the excess of diagnosis). And all this with only four shots of biopsy, compared with 12 shots of biopsies traditional with the ultrasound.
These findings should lead to a change for the patients on the pathway in the diagnosis of early prostate cancer in two ways:
1. All patients with a clinical suspicion of prostate cancer should provide a magnetic resonance imaging as part of its way of making decisions before the biopsy.
2. Should be offered a biopsy of the merger to all patients with an anomaly in its Resonance.
A reason of concern, as are patients with a normal mri (28% of patients), despite clinical suspicion of prostate cancer, did not have a biopsy. How many cancers clinically significant could lose by not offering a biopsy these patients? An answer of what we would find, the offers studio PROMIS (Prostate MR Imaging Study) that included a biopsy extensive for patients with an Mri normal.
In the study PROMIS, the negative predictive value of Mri to detect any type of cancer 4 is 76%, that is to say, up to 1 in 4 men will have cancer of pattern 4 in the transperineal biopsy. However, it is not lost in the primary cancers of the pattern 4 on MRI. You could accept the absence of some cancers of Gleason pattern 4 in some men, provided that the “routine follow-up” is appropriate.
This could provide sufficient evidence to adopt fully the indication of the Resonance in the approach for the early detection of prostate cancer. Based on the study PROMIS, published in The Lancet in 2017, in addition to the study, the PRECISION, the results provide the knowledge to fully integrate the magnetic resonance imaging in the evaluation of men with suspicion of prostate cancer. The era of prostate biopsy blind randomised possibly have done, except perhaps in those patients in whom Mri is contraindicated.
Genetic markers
The genetic marker SelectMDx helps to prevent the realization of prostate biopsies unnecessary. This study is performed on a urine test, is a non-invasive study for the detection of the risk of having aggressive cancer of prostate.
The marker genetic ConfirmMDX for prostate cancer addresses the concerns of a prostate biopsy with a false-negative result.
The test ConfirmMDX for prostate cancer addresses the concerns of a biopsy with a false negative, and helps the urologist to:
- DISMISS men who do not have prostate cancer so that they do not undergo biopsies repeated and unnecessary.
- INCLUDE men with high-risk that may need to be repeated with a biopsy, and undergo a possible treatment.
– Diagnosis –
The prognosis and treatment options depend on the following:
- The stage of the cancer (whether it affects part of the prostate, which involves the entire gland or has spread to other parts of the body).
- The age and general health of the patient.
- If the cancer is newly diagnosed or has come back after having been treated and appearance curing.
How do you set the Gleason grade?
The pathologist assesses two areas or zones of the sample of prostate tissue obtained by biopsy of the prostate. Try to choose areas that are well representative of the tumor. Each of the two areas will be assigned a score ranging from 1 to 5.
The 1 corresponds to the cases of low aggressiveness of the tumor (groups of cancer cells resemble the normal glands of the prostate). 2 to 4 are included intermediate situations, progressively aggressive. To set the Gleason grade of each case, add the numbers assigned to each area. For example: 3+ 4=7. Therefore, there is no Gleason score, Or 1, the minimum is 2 (1 + 1). The lower the Gleason score, the lower the possibility that prostate cancer is aggressive, it will grow more slowly and will spread less. On the opposite side, the higher the Gleason score, the more likely aggressiveness of the tumor. In summary, the Gleason located between 2 and 4 correspond to low aggressiveness; the 5 and 6 are intermediate situations and aggressiveness will increase from 7 to 10.
Diagnosed with prostate cancer, tests to be carried out to determine if the cancer cells have spread within the prostate or to other parts of the body of the patient. This process is called classification by stages (or staging). It is necessary to know the stage (or stage) of the disease in order to plan the treatment best suited.
To determine the stage of the prostate cancer is generally indicate:
- Bone scan or body bone scan with radionuclides: Procedure to determine the presence of rapidly dividing cells in the bone, such as cancer cells.
- Scanning by Computed Tomography (CT) para evaluar la presencia de ganglios afectados en el abdomen y la pelvis.
- PET-PSMA Gallium: A procedure that adds the advantages of Tomography Computed to the Nuclear Medicine by increasing the Sensitivity and specificity of previous methods.
The stage of the cancer is based on the results of the staging and diagnostic tests such as biopsy of the original tumor. The biopsy is used to determine the Gleason score.
The cancer spreads in the body in three ways:
- Through the tissue. The cancer invades the normal tissue that surrounds it.
- Through the lymphatic system. Cancer invades the lymph system and travels through the lymph vessels to other places in the body.
- Through the blood. Cancer invades the veins and capillaries and travels through the blood to other places in the body.
When cancer cells are separated from the primary (original) tumor and travel through the lymph or blood to other places in the body, it can form another tumor (secondary). This process is called metastasis. The secondary tumor (metastatic) is the same type of cancer as the primary tumor. For example, if prostate cancer spreads to the bones, the cancer cells in the bones are actually prostate cancer cells. The disease is metastatic prostate cancer, not bone cancer.
STAGES:
Stage I
The cancer is restricted to the prostate. Cannot be felt during a digital rectal exam and is not visible by using a test image. It is often found incidentally during surgery for other reasons, such as benign prostatic hyperplasia. The Gleason score is low. Prostate cancer in stage I may also be called cancer of the prostate in stage A1.
Stage II
The cancer is more advanced than in stage I, but still has not spread outside of the prostate. The Gleason score can vary from 2-10. Prostate cancer in stage II can also be called stage A2, stage B1 or stage B2.
Stage III
The cancer has spread beyond the outer layer of the prostate to nearby tissues. Can you find cancer in the seminal vesicles. The Gleason score can vary from 2-10. Prostate cancer-in stage III may also be called cancer of the prostate in stage C.
Stage IV
The cancer has metastasized (has spread) to the lymph nodes nearby and not close to the prostate to other parts of the body, such as the bladder, rectum, bones, or lungs. Prostate cancer tends to spread to the bones. The Gleason score can vary from 2-10. The cancer of the prostate stage IV can be called also cancer of the prostate in stage D1 or D2.

TREATMENTS
Patients who are in good health, in general they have been offered a treatment with surgery for prostate cancer, being the most recommended Radical Prostatectomy.
Pelvic lymphadenectomy
Surgical procedure in which are extracted from the lymph nodes of the pelvis. The pathologist looks at a tissue sample under a microscope to look for cancer cells. If the nodes contain cancer, the doctor will not remove the prostate and may recommend another treatment.
OPEN RADICAL PROSTATECTOMY
This surgical procedure has been used most often to ablate the prostate, surrounding tissue and seminal vesicles. There are different types of open radical prostatectomy:
► Retropubic prostatectomy
Surgical procedure to remove the prostate through a cut (incision) in the abdominal wall. Given that radical prostatectomy is a surgical intervention radical, it is possible that patients need to receive blood transfusions. Patients typically stay interned approximately 5 days. The probe of the bladder remains placed between two and three weeks, and full recovery can take up to 12 weeks.
► Complications typical of the prostate surgery to open sky
The most frequent complications when a patient should undergo prostate surgery conventional are: impotence, urinary incontinence, bleeding and post-operative care.
The adverse effect most significant long-term conventional surgery is incontinence of urine, which is the inability to control urine flow or partial capacity to contain the flow of urine characterized usually by loss of urine when you cough or make an effort that requires the use of cloths.
► Perineal prostatectomy
Surgical procedure by which the prostate is removed through an incision (cut) is made on the perineum (area between the scrotum and the anus). The lymph nodes may also be removed through a separate incision in the abdomen.
In addition, we practice the following types of surgery:
► Laparoscopic Radical Prostatectomy
This technique is performed through 5 small incisions in the abdomen. Laparoscopic radical Prostatectomy is an established and accepted treatment for localized prostate cancer.
This surgical technique is performed according to the principles of open surgery but without the hand of the surgeon between the patient's abdomen. The lens of the laparoscope, connected to the camera projecting to the monitor with an excellent image to expand the details of the prostate. Once the prostate is separated from the neighbouring organs, is placed in a plastic bag and is extracted through one of the holes created to perform the intervention. The bladder is “re-joined” to the urethra to restore the continuity of the urinary tract with the use of laparoscopic techniques.
The stay is usually 3 to 5 days, during which it is necessary to wear a catheter for 10 days or more to empty the bladder and allow for proper healing of the connection urethra-bladder.
► Pelvic lymphadenectomy
Surgical procedure in which are extracted from the lymph nodes of the pelvis. The pathologist looks at a tissue sample under a microscope to look for cancer cells. If the nodes contain cancer, the doctor may recommend another treatment.
► Prostatectomy Robotic Da Vinci Xi
The da Vinci surgical system provides surgeons with an alternative to both traditional open surgery like laparoscopy, conventional, putting the surgeon's hands at the controls of a robotic platform of the latest generation. The Robot da Vinci Xi allows surgeons to perform even more complex repairs and delicate by using very small incisions with unmatched precision, improving the skill of the surgeon and optimizing their results.
Translates the surgeon's movements in an intuitive way, allowing full control of the optical fiber and of the instruments, avoiding the complex movements laparoscopic;
Allows a glimpse into real three-dimensional of the operative field: the surgeon enters, literally, in a process of "immersion", in order to assess the best possible planes of dissection, anatomical and "live" the surgical intervention, almost from within the body of the patient.
For prostate cancer incorporates the best techniques of traditional surgery and applies it to a method of minimally invasive robot assisted.
Watchful Waiting
Is the intensive observation attentive to the condition of the patient without administering any treatment until symptoms develop or change. It is usually used in men suffering from other medical problems and with a disease stage that is just beginning.
Radiation therapy
Radiation therapy is used to treat prostate cancer. Are the radiation treatment, is a general term used to describe several types of treatments, including the use of high power X-ray, the introduction of radioactive materials into the body, or the injection of substances in the blood stream.
Different types of radiation therapy:
Radiation therapy external beam (EBRT, for its acronym in English): it is the most common type of radiation therapy. These X-rays destroy tumor cells by damaging their DNA. During treatment, the radiation exposure is brief and non-invasive, so patients feel no discomfort during exposure to radiation.
External radiation therapy is usually given once per day, five days a week. The primary treatment for localized cancer of the prostate typically requires about eight weeks of treatment.
The usual side effects of the use of EBRT for prostate cancer include increased urinary frequency; mild burning when you urinate; weak urinary stream; irritable bowel with mild diarrhea, gas, urgent need to defecate and gut sensitivity; mild skin irritation around the rectum; decrease in blood cells, and fatigue.
Among the complications are rare, it includes the bleeding rectal important, the irritability of the bladder and urethral stricture. Another side effect away relatively common radiation is the loss of the erection, and depends on the use of other treatments, such as hormonal treatments and the presence of other diseases that may affect sexual function.
Conformal radiotherapy 3D
The conformal radiotherapy 3D decomposes schematically in 3 stages; the acquisition and processing of images in 3 dimensions, the planning and finally the execution and verification of the treatment. There are limits and uncertainties throughout this entire process that what other technologies are used in constant evolution. The delineation of the volume target and the organs at risk, crucial stage of the conformal radiotherapy 3D, can be variable between one professional and another. The margins of safety around these volumes that have in mind the internal movements of the organs and the uncertainties of the tumor extension, they are still empirical, and may, again, be any different between one computer and another.
There are, however, the consensus among radiation oncologists and medical physicists to recognize the conformal radiotherapy 3D as a technique with more precise and elaborated than the conventional radiotherapy. The comparison of the plans available showing a decrease of the radiation dose in the healthy tissue has been awarded the membership of the profession.
The conformal radiotherapy 3D is visibly less toxic at doses equal to conventional radiation therapy.
Intensity-Modulated radiation therapy
Intensity-modulated radiation therapy (IMRT for its acronym in English) is a modality that uses X-ray accelerators, computer controlled to deliver precise radiation doses to a malignant tumor to specific areas within the tumor. IMRT allows the radiation dose to conform more precisely to the three-dimensional form 3-D of the tumor by modulating-or controlling-the intensity of the radiation beam.
Hace posible enfocar dosis más altas en regiones dentro del tumor; al tiempo que se minimiza la exposición a la radiación en las estructuras críticas circundantes normales.
IMRT has the potential to reduce treatment toxicity, even at doses are not increased. The IMRT does require longer periods of treatment daily and administered a lower dose to larger volumes of normal tissue with conventional radiation therapy.
BRACHYTHERAPY
There are two approaches different to apply brachytherapy in the treatment of prostate cancer: a low rate of dose rate (LDR, for its acronym in English), and high rate of dose (HDR, for its acronym in English).
The prostate brachytherapy is usually applied by using the technique of LDR. With brachytherapy LDR, the seeds are placed permanently in the prostate. The radiation is administered in a gradual manner over a period of months. HDR brachytherapy is performed by placing a source of highly radioactive in the prostate on a temporary basis. The radiation treatment is administered in a few minutes and is repeated two or three times over the course of several days.
A small percentage of patients will suffer a urinary blockage in the weeks following the procedure and will have to use a catheter. Normally, these disappear after a few weeks, and once the swelling is reduced, the tube is removed.
As the radioactive seeds are placed inside the prostate, it is not common to observe intestinal side effects in the short term. However, like the previous part of the rectum is close to the prostate, with the passage of time can occur intestinal side effects similar to those of the EBRT. As with other treatments with radiation, there can be dysfunction sexual erectile.
HORMONE replacement therapy
It is the treatment which eliminates the action of hormones or intercepts your action to stop the growth of prostate cancer. Hormones are chemical substances produced by glands in the body that circulate through the bloodstream. In the case of cancer of the prostate, the male sex hormones can cause the cancer to grow. You can use medications, surgery, or other hormones to reduce the production of male hormones, or prevent them from exercising their function.
The hormone replacement therapy used in the treatment of prostate cancer may include the following substances:
- Agonists of gonadotropin-releasing hormone luteinizing hormone can prevent the testicles from producing testosterone.
- Antiandrogens can block the action of androgens (hormones produced by the male sexual characteristics) as cyproterone, flutamide, bicalutamide and nilutamide.
- Medications that can prevent the adrenal glands produce androgens include ketoconazole and aminoglutethimide.
- The orchidectomy is a surgical procedure that is performed to remove both testicles, the main source of male hormones, in order to reduce the production of these hormones.
- Estrogens (hormones produced by the female sexual characteristics) can prevent the testicles from producing testosterone. However, estrogens are rarely used in the treatment of prostate cancer because of the risk of dangerous side effects.
Men treated with hormone replacement therapy you can submit: blush, impairment of sexual function, loss of sexual appetite, and weakness in the bones.
Other treatments
CRYOSURGERY
The treatment uses needles, ultra thin, using sophisticated technology, creates a sphere of ice in the interior of the prostate gland that reach temperatures of ultra freezing at -70 ° C, destroying the tissue of the prostate cancer and its content.
A combination of gases argon and helium, allows you to control the temperature. The argon gas flowing through the needle generates a very low temperature causing the formation of ice. It takes advantage of the creation of spheres of ice with precision to create a region of freezing, which fits exactly the size and shape of the prostate. The process of freezing is lethal to the cells, and ends with the entire prostate tissue.
Cryosurgery of the prostate is the entire prostate and your objective is to freeze the prostate tissue. In this process, the nerves responsible for erection of the penis may be affected, and, as with surgery and radiation therapy, erectile dysfunction is a potential complication of this treatment.
CHEMOTHERAPY
Cancer treatment that uses drugs to stop the growth of cancer cells, by removing them or preventing their multiplication. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy).
When chemotherapy is placed directly into the spinal column, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
The way the chemotherapy is given depends on the type and stage of the cancer being treated. Combination chemotherapy is the treatment with the use of two or more anti-cancer drugs.
BIOLOGICAL THERAPY
Treatment that uses the patient's immune system to fight cancer. Substances made by the body or in the laboratory are used to boost, direct or restore the body's natural defenses against the cancer. This type of treatment of cancer is known as biotherapy or immunotherapy.
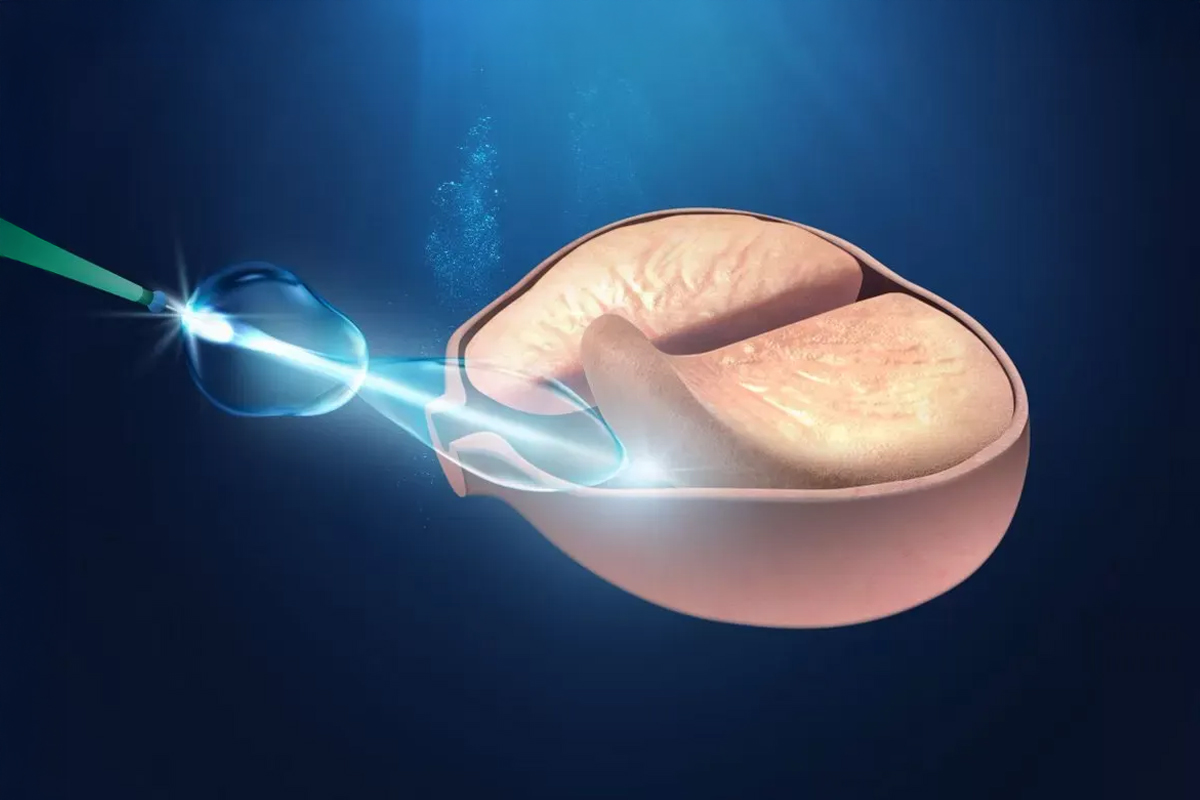
Ultrasound concentrated, high-intensity (HiFu)
It is a medical device addressed by a computer, designed to treat localized cancer of the prostate, using high-intensity focused ultrasound. The energy is released from an endorectal probe. The ultrasonic waves travel through the walls of the rectum without damaging it, and are focused on the prostate. This focusing produces an intense heat and instant that causes irreversible destruction of the selected area, without damaging the surrounding tissues.
This therapeutic option is aimed at patients in first intention or as salvage after failure of radiation therapy.
Lea tambien sobre Enlarged prostate: symptoms, treatment and home remedies