Symptoms
Testicular cancer usually occurs in young men 15 to 35 years. This is the most common cause of cancer in patients younger men. It is important to note that the testicular cancer has a great potential for healing.
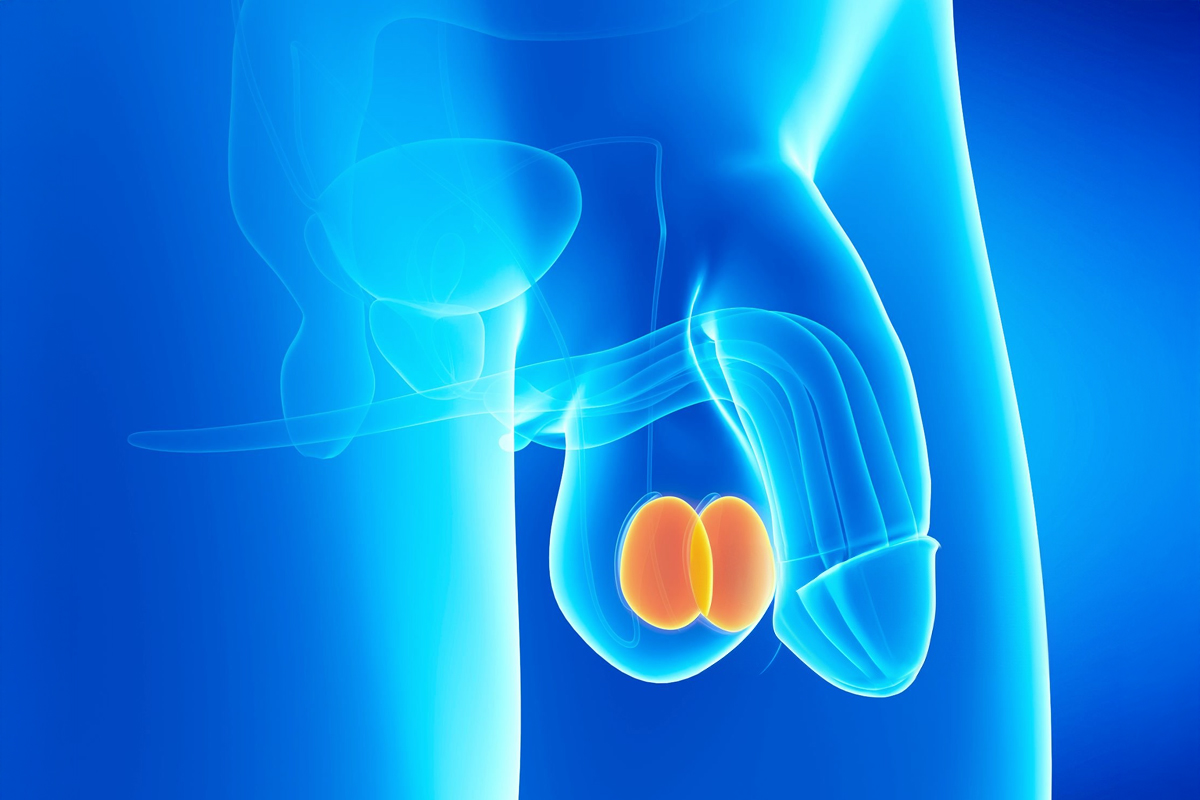
The testes are the organs pairs of genital system male, they produce male sex hormones and sperm for reproduction.
Usually, the majority are detected by a induration in any of the testis. As tends to be painless and without inflammatory reaction, patients do not prioritize the query. Some of the symptoms most common:
- A lump or enlargement in either testicle.
- A feeling of heaviness in the scrotum.
- Pain in the abdomen or in the groin.
- Sudden buildup of fluid in the scrotum.
- Pain or discomfort in a testicle or in the scrotum.
- Enlargement or tenderness in the breasts.
- Back pain.
Causes
Testicular cancer occurs when healthy cells in a testicle alter. Healthy cells grow and divide in an orderly way to maintain the normal functioning of the body. Sometimes, some cells exhibit abnormalities and this makes this growth is getting out of control, generating cancer cells that form a mass in the testicle.
Risk factors
- Testicular development is abnormal: for example, undescended testes (when the testicles have not descended normally into the scrotum), among other testicular abnormalities.
- Previous testicular cancer.
- Family history.
- Age.
Diagnosis
Usually, the physical examination confirms the diagnosis; adicionalment the Urologist will ask you for a testicular ultrasound, will provide analyses of blood, may indicate a chest x-ray and computed tomography of the abdomen and pelvis with contrast, or a magnetic resonance imaging to confirm the diagnosis.
Treatment
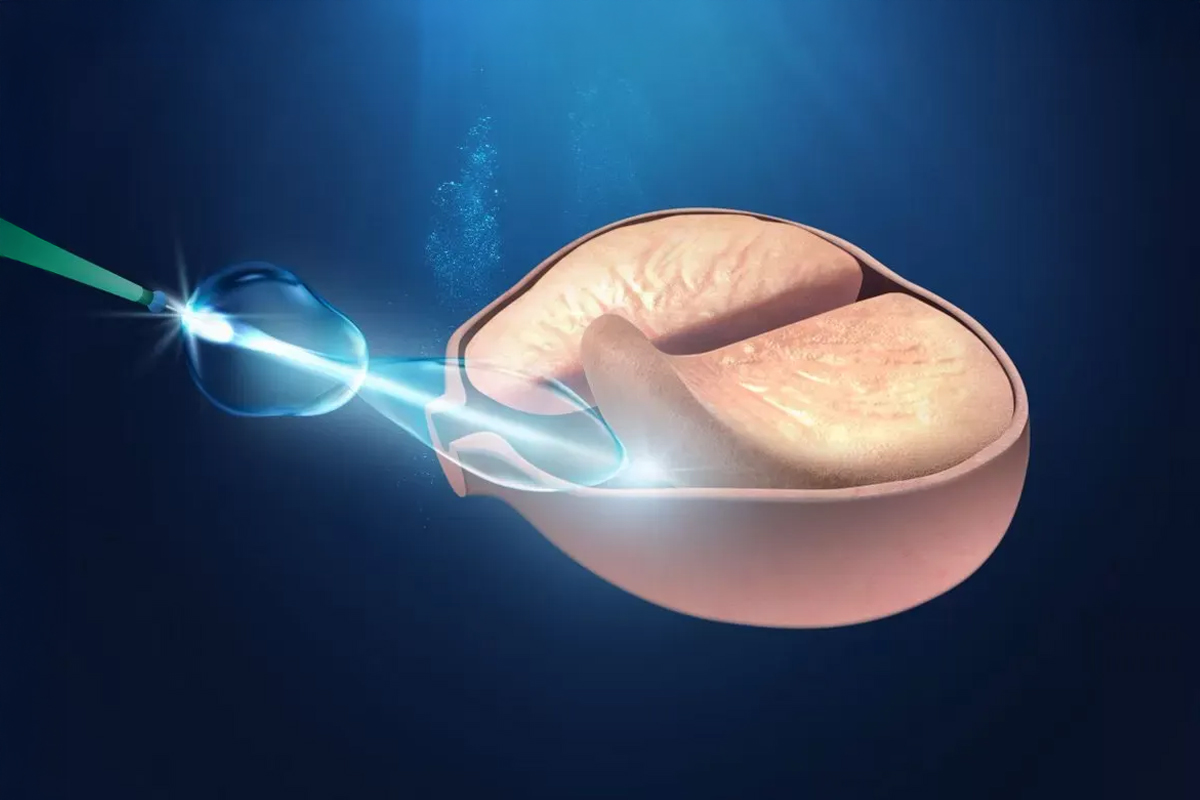
Usually, surgery is necessary, the Urologist will decide at that time if it is necessary to perform an intraoperative biopsy before deciding to remove the testicle. The surgery consists of the excision of the entire testis, the epididymis and the spermatic cord to send the entire analysis.
Can be placed at that time a testicular prosthesis for aesthetic purposes.
The Medical Pathologist will establish what type of tumor it is. In most of the cases the histological type is called tumors seminomatosos, the other tumors are called no seminomatosos. This result will be analyzed with the Urologist to determine the treatment after the surgery. This treatment varies according to the type of tumor and stage of the same. The options are:
- Control or monitoring: They perform periodic checks with tumor markers and imaging studies with computed tomography or mri, nuclear magnetic.
- Lymphadenectomy retroperitoneal: In some cases, especially in nonseminomas may indicate the removal of the lymph nodes in the retroperitoneum. This technique can be performed to stage the disease or with purpose healing.
- Chemotherapy.
- Radiation therapy retroperitoneal.
The removal of unilateral testicular does not cause hormonal disorders, since it is compensated for by the other testicle. Could be an alteration of the quality of the sperm, this, that, in general, improves with time. In patients who will be undergoing chemotherapy and radiation therapy, it is advisable to obtain semen samples for sperm bank, since this treatment affects the production of sperm, which usually improves after 2 years of treatment.
Prevention
There's No way to prevent testicular cancer. However, it is of great help to the self. Just as women with the self-examination breast, men should be aware that a testicular self-examination might lead to a consultation time with your doctor Urologist to determine the behaviors most appropriate, as the case may be, to follow.
When to consult the doctor?
Consulting the doctor if you notice pain, swelling or lumps in your testicles or groin area, especially if these signs and symptoms last for more than two weeks.