Urinary incontinence is the loss of urine involuntarily. It is a frequent problem, which often causes discomfort in the sufferer. It affects both men and women.
The intensity of the loss of urine is extensive, since it covers from losing urine occasionally when you cough or sneeze to having an urge to urinate so sudden and strong you don't reach the bathroom in time.
Usually, it most commonly occurs in women after pregnancy, in men after surgery prostate and as people get older; however, urinary incontinence is not an inevitable consequence of aging. There are also some external factors such as foods, drinks, and medications that can act as diuretics and cause urinary incontinence in a transitory way. Examples of them are: alcohol, caffeine, soda, and sparkling mineral water, artificial sweeteners, chocolate, foods with a high content of spices, sugar or acid, especially citrus fruits, medicines for blood pressure and the heart, sedatives, and myorelaxants and/or large doses of vitamin C.
In the majority of patients, some changes in the life style or medical treatment can ease discomfort or stop urinary incontinence.
Symptoms
Some patients suffer loss of urine minor and occasional, and by contrast, other patients may present with loss of mild to moderate with greater frequency.
There are different types of urinary incontinence:
- Stress incontinence: urine leaks when you exert pressure on the bladder, such as coughing, sneezing, laughing, exercising or lifting something heavy.
- Urge incontinence: it manifests with a sudden need and intense urges to urinate, followed by an involuntary loss of urine. It is likely that this patient need to urinate often, including throughout the night. It can be caused by several conditions, such as infection, increase in size of the prostate, or systemic diseases, such as those that affect the nervous system and/or diabetes.
- Overflow incontinence: the patient presented with dribbling of urine, frequent or constant because the bladder does not empty completely.
- Incontinence functional: is given by a physical or mental impairment , which prevents the patient arrives at the bathroom in time. For example; if you have severe arthritis, you may not be able desabotonarte the pants quickly.
- Mixed incontinence: is given in those patients who present more than one type of urinary incontinence.
Another type of incontinence is the Bedwetting, which is the involuntary loss of urine that occurs when the patient is asleep.
Diagnosis
The importance of identifying the type of urinary incontinence that the patient has, is due to the good choice of your treatment, as this is fundamental to achieve good results.
The information of the symptoms will serve to guide the treatment decisions that the Urologist told her to. To do this, the Doctor will need an in-depth review of the clinical history of the patient, accompanied by a physical examination, where they will probably ask you to do a maneuver simple that can demonstrate incontinence, such as, for example coughing.
May become necessary complementary studies, such as laboratory or images to complete the diagnosis. If more information is needed, the doctor may recommend tests that are more complex, such as a cystoscopy, a uro-dynamic study, among others.
Treatment
The treatment proposed by the Urologist, will depend on the type of incontinence the patient present. Currently, the treatments offer a variety of options, from therapies kinésicas, the drugs, the electromagnetic energy to stimulate the deep muscles of the pelvic floor (EMSELLA), minimally invasive surgeries and surgeries conventional.
The Urologist will define the treatment of urinary incontinence depending on the type of incontinence of the patient.
It is likely that the patient with a combination of treatments. For example:
- Bladder training, to prolong the time of urinary retention between the current needs to go pee.
- Urinating two times, which means to urinate and wait for a few minutes to re-do it.
- Scheduled hours to urinate.
- Change of habits, as to limit or avoid alcohol, caffeine and acidic foods, to reduce the consumption of liquids, lose weight, and physical activity.
Drugs
There are various treatments available to aid in the management of urinary incontinence:
- Treatments that relax the muscles in the bladder, helping to reduce the frequency and urgency of going to the bathroom.
- Options that contribute to increase the capacity of the bladder to retain urine.
- Treatments aimed specifically at men, which help to reduce the tension in the muscles of the bladder neck and prostate to enhance bladder control.
- Topical therapies of support, especially in women, that can help tone and rejuvenate the tissues of the urethra and the vaginal area.
.
Surgeries
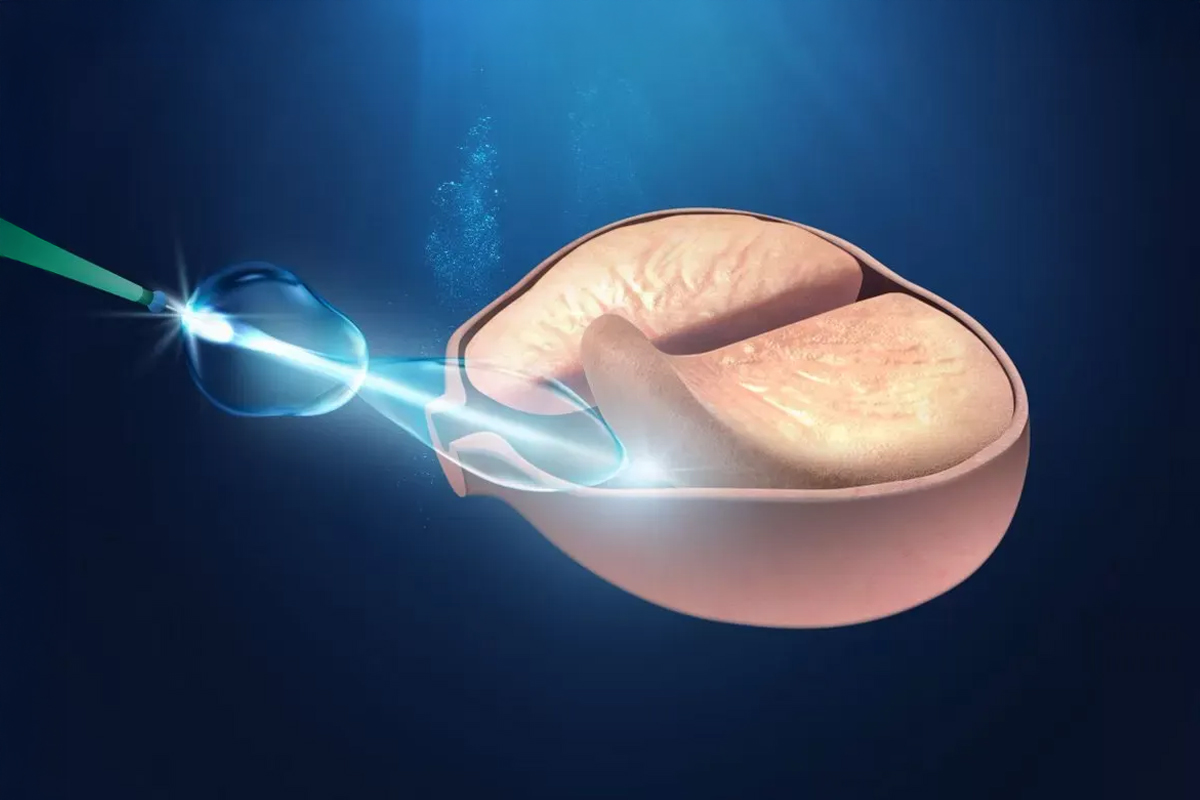
- Injection of filler material: It is injected with a synthetic material in the tissue that surrounds the urethra to keep the urethra closed. Usually, this procedure must be repeated periodically.
- Injection in the muscle of the bladder: May be beneficial for people who have overactive bladder.
- Stimulator nervous: implants a small device, similar to a pacemaker under the skin , it emits electrical pulses to the nerves involved in the control of the bladder
- Procedures with sling: use a synthetic material or a mesh that allows you to keep the urethra closed. .
- Prolapse surgery or suspension of the bladder neck.
- Artificial urinary sphincter: it is used in men, implanted a small ring full of fluid around the neck of the bladder to maintain a closed urinary sphincter until you are ready to urinate.
Kegel exercises to strengthen the muscles of the pelvic floor.
The Urologist may suggest that you do these exercises frequently throughout the day to strengthen the muscles that help control urination. It is likely, that the Urologist will suggest that you work with a physical therapist to help you identify and contract the correct muscles.
EMSELLA
It is a procedure, non-invasive, during which patients remain fully clothed and sitting on the chair EMSELLA. One session with this team provides thousands of contractions such as Kegel exercises.

The treatment helps patients to regain control over your bladder, the pelvic floor muscles and to eliminate urinary incontinence. Since this is the only procedure that focuses on the muscles of the pelvic floor and through the technology HIFEM®* cause a profound stimulation in the area of the floor of the pelvis.