Changes in the paradigm for the diagnosis of prostate cancer.
El reciente estudio denominado PRECISION (Prostate Evaluation for Clinically Important Disease: Sampling Using Image-Guidance or Not?), publicado en la prestigiosa revista The New England Journal of Medicine, ha generado un impacto significativo en la forma en que se diagnostica el cáncer de próstata.
Diseño del estudio y población analizada
Se trata de un estudio internacional que incluyó a 500 hombres con sospecha de cáncer de próstata debido a un aumento del PSA (Antígeno Prostático Específico). Los participantes fueron divididos aleatoriamente en dos grupos para comparar diferentes métodos diagnósticos.
Grupo 1: Diagnóstico tradicional
A los pacientes del primer grupo se les aplicó el método convencional: una biopsia prostática transrectal guiada por ecografía, que consistió en la toma sistemática de 12 muestras del tejido prostático.
Grupo 2: Diagnóstico basado en imágenes
En el segundo grupo, en cambio, se utilizó una estrategia diagnóstica basada en los hallazgos de una Resonancia Magnética Nuclear Multiparamétrica de próstata (RMNmp).
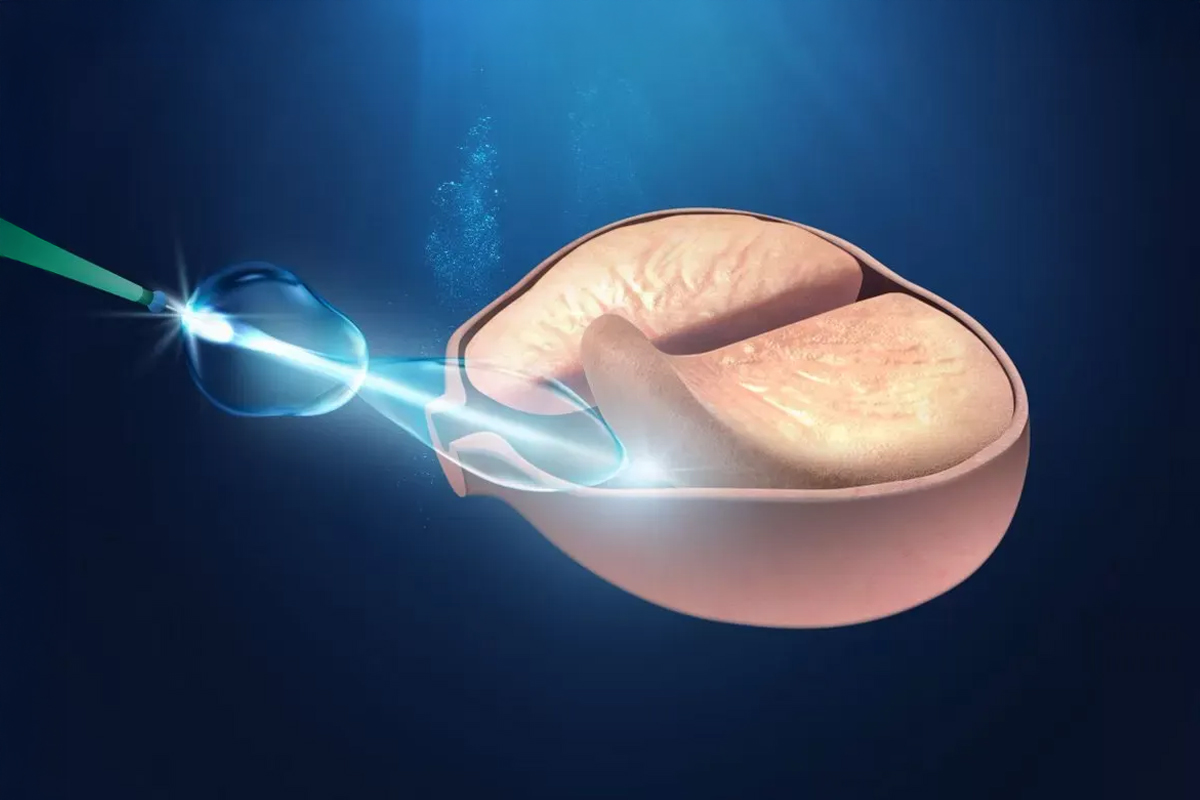
Biopsia dirigida por FUSIÓN
Si la resonancia mostraba resultados anormales, se procedía a realizar una biopsia dirigida por FUSIÓN. Este método combina las imágenes obtenidas por resonancia con las de ecografía mediante un software especializado, permitiendo tomar muestras únicamente de las zonas sospechosas detectadas previamente.
Ventajas del enfoque basado en imágenes
Este enfoque no solo mejora la precisión del diagnóstico, sino que también reduce el número de biopsias innecesarias y sus posibles complicaciones.

Objetivo del estudio PRECISION y resultados clínicos
El objetivo primario de este estudio fue evaluar la tasa de detección de cáncer de próstata clínicamente significativo. Como objetivos secundarios, se consideró la detección de cáncer clínicamente insignificante, definido como enfermedad localizada con volumen tumoral menor a 0,5 cm³, Gleason 6, y sin indicación de tratamiento.
A pesar de que más de una cuarta parte de los hombres evaluados mediante Resonancia evitaron la biopsia, la tasa de detección de cáncer clínicamente significativo fue significativamente mayor en este grupo. Además, la detección de cáncer clínicamente insignificante fue considerablemente menor, reduciendo el sobrediagnóstico. Todo esto se logró con solo cuatro muestras, frente a las 12 utilizadas en el método tradicional guiado por ecografía.

Implicancias clínicas y recomendaciones
Estos resultados sugieren una transformación en el abordaje diagnóstico del cáncer de próstata temprano:
- A todo paciente con sospecha clínica de cáncer de próstata debería ofrecérsele una resonancia magnética antes de la biopsia.
- Si se identifican anomalías en la resonancia, se debería realizar una biopsia por fusión.
Consideraciones ante una resonancia normal
Un aspecto crítico es qué hacer con los pacientes cuya resonancia resulta normal (28% en el estudio), pese a la sospecha clínica. ¿Cuántos casos clínicamente significativos podrían pasarse por alto al omitir la biopsia?
El estudio PROMIS (The Lancet, 2017) aporta información valiosa al respecto. En pacientes con resonancia normal, el valor predictivo negativo fue del 76% para detectar cualquier cáncer, lo que implica que 1 de cada 4 hombres aún podría tener un cáncer de patrón 4. Sin embargo, la RMN no pasó por alto los cánceres primarios de ese patrón. Aun así, con seguimiento adecuado, podría aceptarse el riesgo de omitir ciertos cánceres Gleason 4 en determinados casos.
Comparación entre métodos: datos de detección
- Grupo 1 (biopsia tradicional guiada por ecografía):
- Cáncer clínicamente significativo: 26%
- Cáncer clínicamente insignificante: 22%
- Grupo 2 (biopsia por fusión con RMNmp):
- Cáncer clínicamente significativo: 38%
- Cáncer clínicamente insignificante: 9%
Estos datos respaldan firmemente la integración sistemática de la resonancia magnética en la evaluación de pacientes con sospecha de cáncer de próstata. La era de la biopsia sistemática aleatoria podría estar llegando a su fin, salvo en casos donde la RMN esté contraindicada.